It was late on a busy ward when a missing infusion pump delayed a procedure. Nurses searched hallways and closets while the patient waited. That short delay showed how device visibility affects patient care and staff stress.
![]()
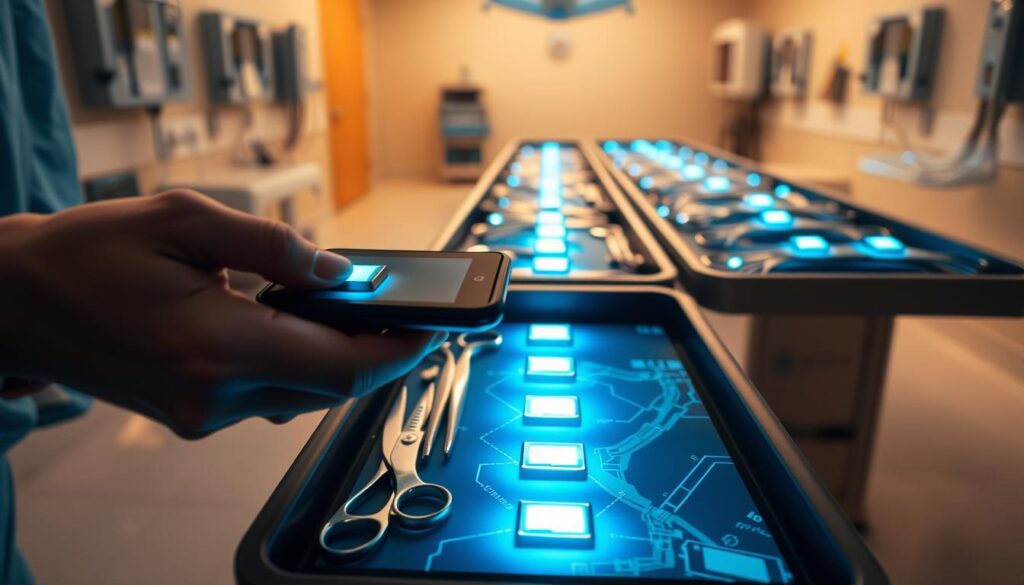
This guide helps hospital leaders choose between RFID and BLE for equipment locating and workflow gains. We compare room‑level BLE accuracy to within 1–3 meters and the rapid, high‑volume audits that passive RFID can deliver.
Expect clear guidance on cost, scale, accuracy, integration with clinical systems, and ROI. Iottive brings hands‑on experience building BLE apps, cloud/mobile platforms, and end‑to‑end IoT solutions for healthcare teams.
Key Takeaways
- BLE gives room‑level location; passive RFID excels at fast audits.
- Choosing depends on device type, mobility patterns, and budget.
- Integrations reduce wasted time and lower rental or replacement costs.
- Scale considerations matter when moving from one ward to multi‑facility.
- Iottive offers healthcare-ready BLE and IoT platforms to support deployment.
Choosing the right tech today: RFID or BLE for hospital asset tracking
Hospitals must weigh high‑volume audit speed against room‑level real‑time visibility when selecting a solution.
Use case matters: passive rfid best serves fast audits, PAR checks, and storeroom sweeps where many items are read at once. BLE excels for frequent location updates of mobile devices and equipment that move between wards.
Facility layout and materials affect performance and costs. Dense walls or long corridors can increase gateway or reader counts. Plan infrastructure around room density and throughput needs.
Data cadence is a key difference. BLE delivers continuous, near‑real‑time location (often 1–3 meters with sufficient gateways). rfid provides event‑based reads at chokepoints and during scheduled audits.
Operational goals—cutting search time, lowering rentals, and improving care coordination—should drive selection. Integrate location feeds with inventory and maintenance systems to surface repairs and reduce unnecessary hires and late fees.
For many hospitals a blended, phased approach works best. Start with audits where quick wins appear, then roll out BLE for high‑mobility devices. Iottive helps quantify benefits and design a right‑sized deployment to match budgets and timelines. Contact: www.iottive.com | sales@iottive.com

How RFID and BLE compare for hospital asset management
Choosing the right mix of reads and real‑time updates reduces search time and boosts patient care.
RFID fundamentals: passive vs semi‑passive, readers, and audit workflows
rfid technology uses radio frequency fields to identify rfid tags on equipment. Passive tags are low cost; semi‑passive (BAP) add sensors. Specialized autoclave‑ready tags handle sterilization cycles.
Handheld readers or carts sweep wards for fast audits. Portal readers capture movements at chokepoints. Systems reconcile scans with inventory and maintenance records to flag repairs or losses.
BLE fundamentals: beacons, gateways, and room‑level location
Small beacons attach to devices and fixed gateways triangulate room‑level location. With enough gateways, accuracy is often 1–3 meters. Continuous updates support quick searches and alerts for high‑value equipment.
When to use each: audits vs real‑time lookups
- Use passive reads for large, scheduled inventory checks and compliance.
- Use BLE for frequent lookups of infusion pumps, monitors, beds, and wheelchairs.
- Combine both: periodic RFID counts plus persistent BLE visibility for inventory management and better patient care.
| Component | RFID | BLE |
|---|---|---|
| Main parts | rfid tags, readers, middleware | beacons, gateways, cloud app |
| Data pattern | Event reads at portals or audits | Continuous room‑level updates |
| Best for | High‑volume inventory verification | Frequent lookups of mobile equipment |
| Infrastructure | Readers, chokepoints, scan carts | Gateway placements, network backhaul |
Iottive’s BLE App Development and Cloud & Mobile Integration streamlines beacon and gateway data into maps, search, and alerts that help care teams find medical assets faster and save time.
RFID asset tracking in hospitals
Large inventories demand methods that find items fast and keep supply lists accurate.
Key benefits: reduced search time and better utilization
Rapid audits let staff sweep departments and update inventory quickly. That reduces time spent searching and frees clinicians to focus on patient care.
Visibility across wards lowers unnecessary rentals and helps avoid late return fees. Systems that read thousands of items at once can reveal unused equipment and improve utilization.
“Passive reads can turn hours of searching into minutes, saving staff time and cutting costs.”

Operational considerations: sterilization, maintenance, and compliance
Choose durable rfid tags for general equipment and autoclave‑resistant tags for sterilizable instruments. Place readers at chokepoints—sterile processing and loading docks—to capture movements between departments.
Integrate reads with asset management and maintenance schedules to flag devices due for service. Follow GS1 standards and keep audit trails to meet regulatory reviews.
| Use case | Typical benefit | Notes |
|---|---|---|
| High-volume audits | Faster inventory reconciliation | Low-cost tags enable broad coverage |
| Preventive maintenance | Scheduled servicing flagged | Integrate with CMMS for work orders |
| Loss prevention | Reduced shrinkage and rentals | Visibility across beds, wheelchairs, laptops |
Iottive designs end-to-end IoT solutions and rfid-friendly apps that streamline audits, alerts, and maintenance workflows for healthcare providers.
Accuracy, coverage, and infrastructure demands inside hospitals
Accuracy and coverage shape how well location systems work on clinical floors.
BLE can locate high-value equipment in real time to within 1–3 meters when gateways are placed on ceilings or walls and calibrated for room-level service.
Gateways need reliable power, network backhaul, and an initial calibration sweep. Proper placement reduces false positives and improves location tracking for pumps, monitors, beds, and wheelchairs.

Read ranges, chokepoints, and performance factors
Radio frequency read performance varies with tag type, reader power, antenna tuning, and environment. For passive rfid, optimize chokepoints at entrances, supply rooms, and sterile processing areas to capture bulk reads.
Readers and antennas should be tuned and tested to reduce missed reads. Tag orientation and shelving can affect read rates during high‑volume audits.
Coverage models and operational advice
- BLE: continuous room updates for real-time visibility when gateway density is sufficient.
- RFID: event-based reads that scale economically for many assets and fast audits.
- Integrate both into a single systems view so staff-facing apps and management dashboards show one source of truth.
Start with dense BLE in critical care, pair RFID sweeps for storerooms, and choose hospital‑grade hardware to support sustainable operations. Iottive’s BLE App Development and Cloud & Mobile Integration translate gateway data into floor maps, search, alerts, and APIs for real-time visibility across healthcare workflows.
Total cost, ROI, and scaling from one ward to system‑wide deployment
Budget decisions require a clear split between upfront and ongoing costs. Upfront costs include tags and readers versus beacons and gateways. Ongoing costs cover software licensing, integration, maintenance, and battery replacement.
Upfront vs ongoing costs
- Hardware: readers, gateways, and beacons or tags.
- Software: cloud licenses, dashboards, and APIs.
- Operations: integration, network, and routine maintenance.
Quantifying savings
Use the nurses’ benchmark: ~208 hours per year spent searching. Automating location reduces that time and reassigns it to care. Passive reads cut labor for manual counts, while BLE reduces time to find equipment and avoids rentals and late fees.
Plan device density per floor for required accuracy and factor beacon battery life (multi‑year for devices like SPARROW). Include gateway resilience (KONA Micro battery backup) and cloud failover in TCO.
“A phased pilot validates savings, then scale by ward and facility with measurable ROI milestones.”
| Phase | Key cost items | Primary ROI drivers |
|---|---|---|
| Pilot | Beacons/tags, a few gateways, software fees | Reduced search time, audit efficiency |
| Scale | Expanded gateways/readers, integration, maintenance | Fewer rentals, loss prevention, better utilization |
| Enterprise | Multi‑site network, security, support contracts | System‑wide visibility, lower total costs |
Iottive delivers end‑to‑end IoT solutions, BLE apps, and cloud services to lower implementation costs and accelerate ROI for healthcare. Contact: www.iottive.com | sales@iottive.com
Integration and data flow: from tags to staff workflows
A clear data flow turns raw reads into timely alerts that staff can use at the point of care.
Connecting to CMMS, EHR, and inventory
Automated maintenance links reader events to CMMS for scheduled servicing, calibration alerts, and compliance records. That reduces missed checks and speeds repairs.
Linking EHR and inventory management adds context. Systems can show equipment readiness tied to patient schedules and procedure needs.
Cloud and mobile experiences for staff
Data moves from readers and gateways to cloud tracking software via standardized APIs. Dashboards and BI tools get clean, usable feeds for management reports.
- Mobile maps and fast search by device type or ID.
- Proximity guidance to the nearest equipment and simple status updates.
- Alerts for dwell time, zone breaches, and maintenance due dates.
Data governance and resilience: role-based access, audit trails, PHI avoidance, and gateway battery backup keep systems reliable during outages.
“Iottive’s BLE App Development and Cloud & Mobile Integration accelerates integrations and reduces IT burden.”
Contact: www.iottive.com | sales@iottive.com
From pilot to production: your hospital implementation roadmap
Successful deployments balance technical validation with frontline workflows and safety checks. A clear roadmap keeps disruption low and helps teams adopt new systems fast.
Assessment and site survey: asset classes, risk areas, and infrastructure readiness
Start with a focused assessment. Catalog assets and equipment by class and clinical risk. Identify search hotspots and inventory choke points.
Run site surveys to validate BLE gateway density for target accuracy and reader placement for reliable reads, noting power and network availability.
Pilot design and validation: location accuracy, throughput, and safety protocols
Define KPIs: accuracy targets, audit throughput, time to find equipment, and safety outcomes. Test BLE placement and rfid reader chokepoints under real workflows.
Include infection control rules for tags and mounts. Consider LoRaWAN gateways with battery backup (KONA Micro) and hybrids (SPARROW) for resilience and long battery life.
Training and change management: adoption, policies, and continuous improvement
Build role-based training, quick guides, and help-desk paths for staff. Set governance for tag maintenance and systems ownership per unit.
- Validate CMMS/EHR/inventory integrations during pilot.
- Stage scale-up from ward → units → hospitals, refining placement and policies.
- Use dashboards to monitor time to locate, audit rates, and maintenance compliance.
Iottive provides end‑to‑end IoT/AIoT solutions from site surveys and pilot design to training, rollout, and continuous improvement in healthcare. Contact: www.iottive.com | sales@iottive.com
Why choose Iottive for BLE, RFID, and end‑to‑end IoT in healthcare
Iottive builds practical IoT solutions that let clinical teams find devices fast and reduce wasted time. We combine Bluetooth engineering, cloud apps, and secure mobile UX to deliver measurable results for healthcare clients.
Our expertise spans full lifecycle delivery:
Our expertise: IoT/AIoT solutions, BLE app development, cloud & mobile integration
End‑to‑end capabilities include BLE app development, cloud integration, custom IoT platforms, and system APIs. We provide deployment playbooks, clinical UX design, and secure integrations with CMMS, EHR, and inventory systems.
Healthcare use cases we serve
We help teams manage infusion pumps, beds, wheelchairs, monitors, and IT devices. Our work reduces time to locate equipment, cuts rental and late fees, and lowers loss rates.
| Capability | Benefit | Notes |
|---|---|---|
| BLE & rfid unification | Room updates + fast audits | Maps, search, alerts, analytics |
| Integrations | Automated maintenance | CMMS/EHR/inventory linkage |
| Reliability | Continuous location visibility | Gateway redundancy & battery backup |
Flexible commercial models let hospitals pilot, scale, and measure ROI. To scope your asset tracking solution, schedule a discovery session at www.iottive.com or email sales@iottive.com.
Conclusion
Prioritize solutions that cut search time for nurses and deliver measurable ROI quickly.
Use BLE for continuous, room‑level location tracking of mobile medical equipment and use RFID for scalable, high‑volume audits of tags and storerooms. A blended approach often offers the best coverage across varied device types and floor plans.
Connect tracking software to CMMS, EHR, and inventory management so reads drive maintenance, reduce rentals and late fees, and lower loss. Plan gateway density, battery life, and infection‑control mounts during pilots.
Start small, validate KPIs, then expand across hospital systems with resilient gateways and clear reporting dashboards. Partner with Iottive to scope a right‑sized solution and kick off rapid, measurable gains: www.iottive.com | sales@iottive.com.
FAQ
What are the core differences between RFID and BLE for hospital asset monitoring?
RFID uses radio tags read by fixed or handheld readers and excels at fast, high-volume scans for inventories and audit workflows. BLE relies on battery-powered beacons and gateways to provide continuous, room-level visibility and real-time location of mobile devices like infusion pumps and portable monitors. Choose RFID for rapid audits and BLE when you need live location and staff notifications.
Which technology is better for tracking infusion pumps and other frequently moved devices?
For devices moved often across wards, BLE provides the persistent, near-real-time location that clinicians need to find pumps and start care faster. RFID can supplement BLE by supporting nightly or frequent bulk audits to reconcile inventory and detect losses without installing many battery-dependent tags.
How do read range and accuracy compare between these systems in clinical settings?
BLE typically delivers room-level accuracy around 1–3 meters when gateways are placed correctly. Passive RFID read ranges vary from a few centimeters with handhelds to several meters at choke points with fixed readers, making it ideal for corridor or doorway scans and batch audits rather than continuous room-level tracking.
What infrastructure is required to deploy BLE or RFID across a ward or entire hospital?
BLE needs a grid of gateways or access points with power and backhaul, plus battery-powered tags and a cloud/mobile app. RFID requires readers at chokepoints or handheld units, durable tags, and integration with inventory software. Both need network connectivity, a management console, and security controls to protect patient and device data.
How do costs compare and what affects total cost of ownership?
Upfront costs include tags, readers/gateways, installation, and software. Ongoing costs cover battery replacement for active tags, maintenance, support, and cloud services. BLE often has higher tag costs and battery upkeep but delivers real-time value; RFID can be lower per-tag for passive solutions and cuts audit labor dramatically. ROI depends on savings in nurse time, reduced rentals, and fewer misplaced devices.
Can these systems integrate with CMMS, EHR, or inventory software?
Yes. Modern solutions expose APIs or use HL7/FHIR connectors to push location and maintenance events into CMMS and EHR workflows. Integration enables scheduled maintenance alerts, compliance records, and faster device lookup directly from clinician apps or asset management dashboards.
What operational considerations should I plan for around sterilization and cleaning?
Tags and beacons must be selected for sterilization resistance or placed in protective housings compatible with cleaning agents. Procurement teams should require medical-grade enclosures and validate tag performance after routine disinfection cycles to prevent read failures and ensure patient safety.
How do you measure savings like reduced search time and fewer rentals?
Track baseline metrics: average search time per device, number of rented units, and loss incidents. After deployment, measure reductions in nurse minutes spent searching, decreases in rental invoices, and lower write-offs for missing devices. Translate time savings into labor cost reductions and compare against system costs for ROI calculations.
What are best practices when piloting a location solution before system-wide rollout?
Start with a site survey to map assets, traffic patterns, and signal obstacles. Pilot a representative ward, validate location accuracy and throughput, and test integrations with maintenance and clinical workflows. Collect user feedback, refine tag placement and gateway density, and document SOPs before scaling.
How do you manage battery life and device density for BLE deployments?
Choose beacons with long-life batteries, optimize reporting intervals, and implement remote battery monitoring. Plan density based on device counts per ward and expected movement. Regular maintenance schedules and automated alerts for low battery help keep coverage reliable during multi-facility rollouts.
What compliance and data security measures are essential for these systems?
Ensure encryption for data in transit and at rest, role-based access controls, audit logging, and secure APIs. Adhere to HIPAA where patient-related metadata appears and perform regular vulnerability scans. Vendor contracts should include data residency, breach notification, and support SLAs.
Can a hybrid approach combining RFID and BLE offer advantages?
Yes. A hybrid strategy uses RFID for rapid, high-volume audits and BLE for continuous room-level tracking of critical, mobile devices. This combination maximizes inventory accuracy, reduces search time, and minimizes costs by applying each technology where it performs best.
What hospital use cases benefit most from real-time visibility and alerts?
High-value, time-sensitive equipment such as infusion pumps, ventilators, anesthesia machines, and portable monitors benefit greatly. Real-time alerts reduce delays in patient treatment, prevent duplication of purchases or rentals, and help critical care teams locate devices during emergencies.
How should hospitals plan growth from a single ward pilot to system-wide deployment?
Use pilot data to model device density, gateway and reader placement, and recurring costs. Create phased rollouts by clinical area, align with IT and facilities for power and network readiness, train staff, and establish governance for change management and continuous optimization.
What support should you expect from a vendor during implementation?
Expect site assessment, hardware provisioning, integration services, pilot validation, on-site or remote training, and ongoing technical support. Vendors should provide analytics, dashboarding, and professional services to tune accuracy and reporting for clinical workflows.
